Table of Contents
ToggleWhat They Don’t Tell You About Hysterectomy Regret—and What Women Deserve to Know Before and After Surgery
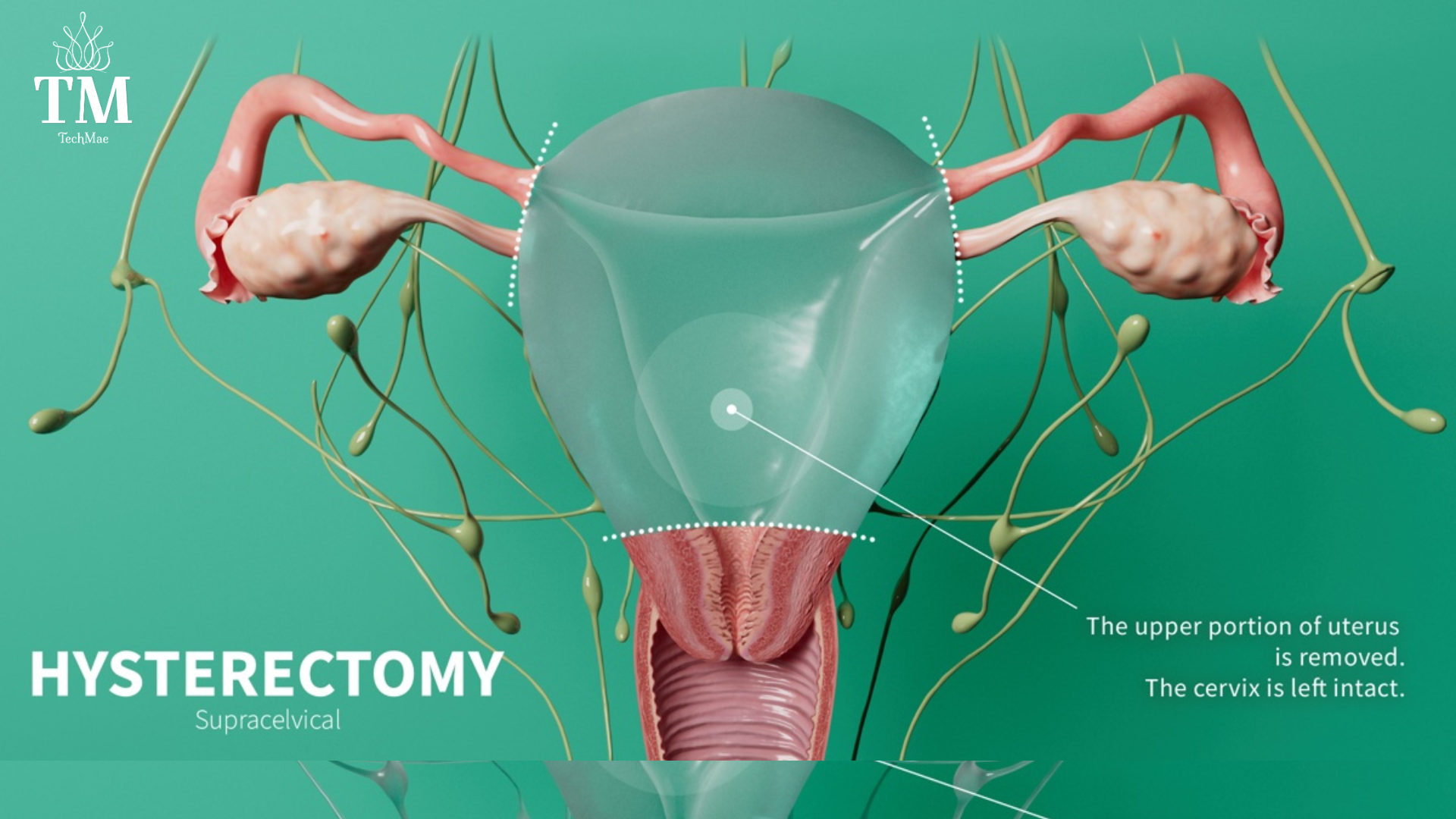
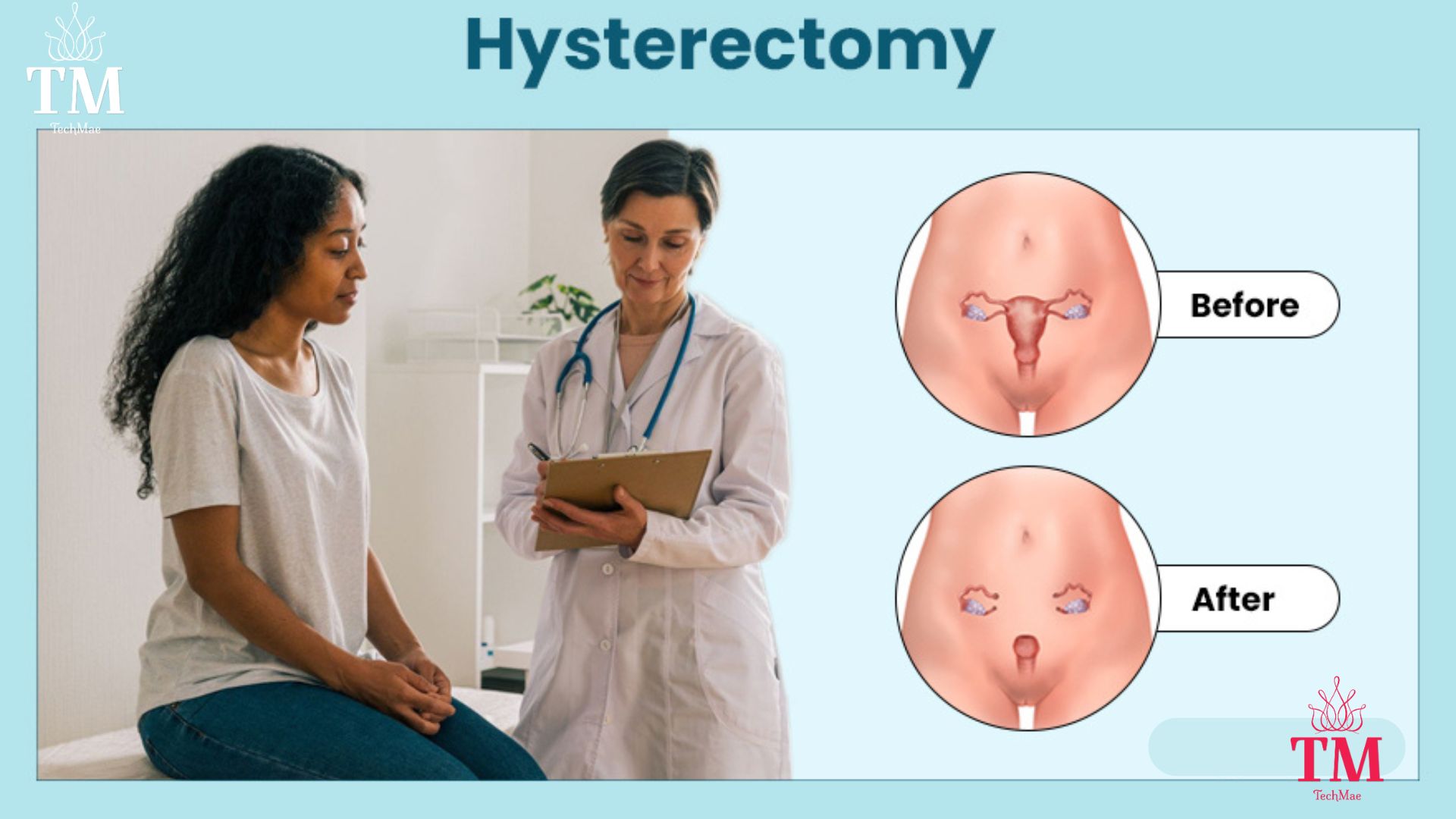
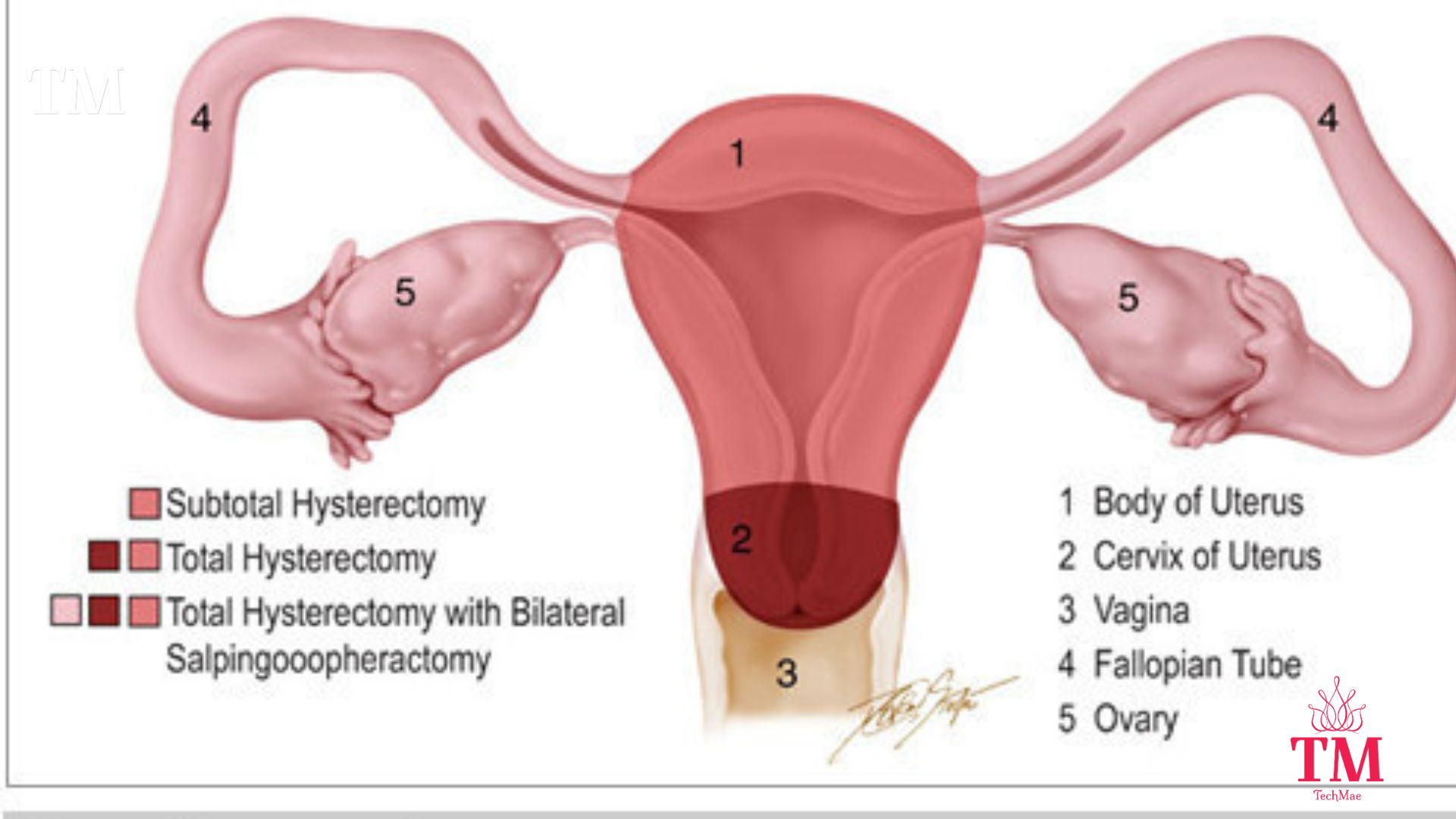
For years, hysterectomies have been offered as a fast-track fix for everything from fibroids to endometriosis to heavy bleeding. But while these procedures are often framed as “routine,” the emotional, hormonal, and long-term consequences rarely make it into the conversation.
Millions of women undergo hysterectomies each year. What’s missing from the operating room, however, is a deeper dialogue—one about identity, loss, trauma, and healing.
It’s time to talk about what so many of us wish we’d known sooner.
What No One Tells You Before Surgery
Too often, women are presented with a script:
-
Done having kids? Remove it.
-
Heavy bleeding? Take it out.
-
Fibroids? Hysterectomy is the gold standard.
But behind the clinical language and quick solutions is a silence around what happens next—when the surgical lights dim and real life begins.
Here’s what many women are not told:
-
Surgical menopause can be instant and intense. If your ovaries are removed, hormone production drops off a cliff. Hot flashes, mood swings, anxiety, and even memory lapses can follow.
-
Sex may feel different—or disconnected. Vaginal dryness, lowered libido, and loss of sensation are common but rarely explained.
-
Mental health can take a hit. Post-op depression, anxiety, brain fog, and a sense of emotional detachment often go unacknowledged.
This isn’t about fear. It’s about informed consent. When we know the full picture, we make better decisions—for our bodies, our minds, and our lives.
Real Talk: Hysterectomy Regret Is More Common Than You Think
In a recent Journal of Women’s Health study, over 40% of women reported regret after their hysterectomy—most citing side effects they didn’t expect.
Here’s what they had to say:
“I didn’t realize how much it would affect my hormones.”
“No one told me I might not feel like myself afterward.”
“I thought I’d be relieved. I just feel empty.”
This isn’t just about anatomy. This is about emotional recovery, identity, and the quiet ways women are left to carry pain they didn’t anticipate.
You Have Options—But You Have to Know to Ask
Not every doctor will present alternatives. Not every woman knows to push for them. And unfortunately, not every voice is heard in the exam room.
If you’re exploring treatment options for fibroids, pelvic pain, or heavy periods, ask about:
-
Uterine Fibroid Embolization (UFE) – A non-surgical, uterus-sparing procedure
-
Endometrial Ablation – Removes the lining of the uterus to reduce bleeding
-
Hormonal IUDs – Can help manage both pain and menstrual flow
-
Functional medicine – Looks at hormonal imbalances from a root-cause level
Holistic Remedies Women Are Exploring for Fibroid Relief
Here are just a few natural paths women are embracing:
- Vitamin D: Low levels have been linked to fibroid growth. Many women report that supplementing improves their cycles, energy, and hormonal balance.
- Soursop (Graviola): A tropical fruit celebrated in Caribbean and African traditions. Its leaves and bitters are used for their anti-inflammatory and healing properties.
- Green Tea (EGCG): Rich in antioxidants that may shrink fibroids over time. Some women take it in supplement form; others drink it daily as part of a wellness ritual.
- Chasteberry (Vitex): A herbal favorite for hormone regulation. Often used to reduce PMS, heavy bleeding, and support estrogen balance naturally.
- Turmeric (Curcumin): A golden anti-inflammatory hero. Women use it in tea, food, or capsules to ease pain and lower inflammation that may worsen fibroid symptoms.
- Flaxseed: Full of lignans that help balance estrogen. Easily added to smoothies or oatmeal, flax supports gentle detox and hormone regulation.
- Castor Oil Packs: A centuries-old practice where warm castor oil is applied to the abdomen to reduce pelvic inflammation and improve circulation. Many women say it’s soothing and grounding—even if not a cure.
These remedies may not replace surgery for everyone—but they are empowering tools for women who want to try natural, low-risk interventions first. Many of these approaches are about restoring balance, managing symptoms, and reconnecting with the body on your own terms.
Healing After the Surgery—Navigating Regret With Grace
If you’ve already had a hysterectomy and feel blindsided by the aftermath, you’re not broken—and you’re not alone.
Maybe you feel empowered.
Maybe you feel disconnected.
Maybe you’re still trying to make sense of the silence.
Whatever your experience, it’s valid.
Here are some ways to begin the healing process:
-
Talk about it—with women who understand
-
Journal through your emotions—grief, anger, relief, confusion
-
Ask about Hormone Replacement Therapy (HRT)—not just for hot flashes, but for mood, libido, and bone health
-
Explore holistic healing—acupuncture, pelvic floor therapy, energy work, herbal support
The road to emotional and physical wholeness after surgery isn’t linear. But it is possible—with the right support.
Healing Is Personal—But It Doesn’t Have to Be Lonely
Whether you’re exploring alternatives or recovering from regret, one thing’s clear: you deserve support.
That’s why inside the TechMae app, we’ve created a private Health & Wellness Community—a space for real conversations about what healing looks like.
Come join women sharing their stories, exploring natural options, and offering wisdom we were never taught but deeply needed.
You don’t have to carry your questions—or your pain—alone.
✨ Download the TechMae app and tap into the collective strength of women healing, learning, and rising together.